The annual Eating Disorder Awareness Week takes place Feb. 24 through Mar. 2, a honorific seven-days spent recognizing the psychological condition that stigmatizes a person’s relationship with food. According to the National Eating Disorders Association, 9% of the United States population will experience an eating disorder in their lifetime. To put that in perspective, that is 28.8 million North American lives put in jeopardy.
There is no “one size fits all” approach to eating disorders as they are complex illnesses that do not discriminate on age, gender, race, or body-size. Actualizing itself in different forms, anorexia nervosa, bulimia nervosa, and binge eating disorder are all prototypes that fall under but are not limited to the eating disorder umbrella. Sudden extreme weight-loss, noticeably low energy levels, and excessive mental occupation of food guilt are examples of red flags that someone could be battling an eating disorder, but they don’t have to fight alone.
When speaking to a loved one over possible concerns about their eating habits, it is essential to approach with a plan. Choosing a safe but private setting to discuss will encourage a peaceful environment, preventing catching them off guard. Alarming the person you are speaking to will only raise tensions causing a decrease in overall rates of comprehension. While the main concern is around their eating disorder tendencies, limit the usage of words relating to weight, food-intake, and body size. This may seem contradictory, but mentioning similar topics could trigger possible feelings of anxiety and end up doing more harm than good.
Instead, utilize “I” statements: “When we are together I am beginning to notice you seem more fatigued than usual, how can I support you?” or “It is alright to feel distressed, I am here for you.” This approach further validates that their struggle is valid, and that you are going to be there to support them through the flames.

Once you have an open understanding of their personal needs, offer to assist them in locating professional support if they are susceptible. It is reasonable to want to “save” your loved one yourself, but you are not a superhero. Rather, having doctorate professionals such as eating disorders specializing therapists and dieticians come into action will have the highest turnout rates for recovery. What you can be is a guiding light—continue to remind the person you care by consistently checking up on them.
If you are struggling, there is help waiting and ready to walk you through the steps of recovery. Organizations such as NEDA (National Eating Disorder Association) and Alliance for Eating Disorders both offer 24 hour national hotlines and assistance to help locate eating disorder specialized treatment that falls under most insurance coverages.
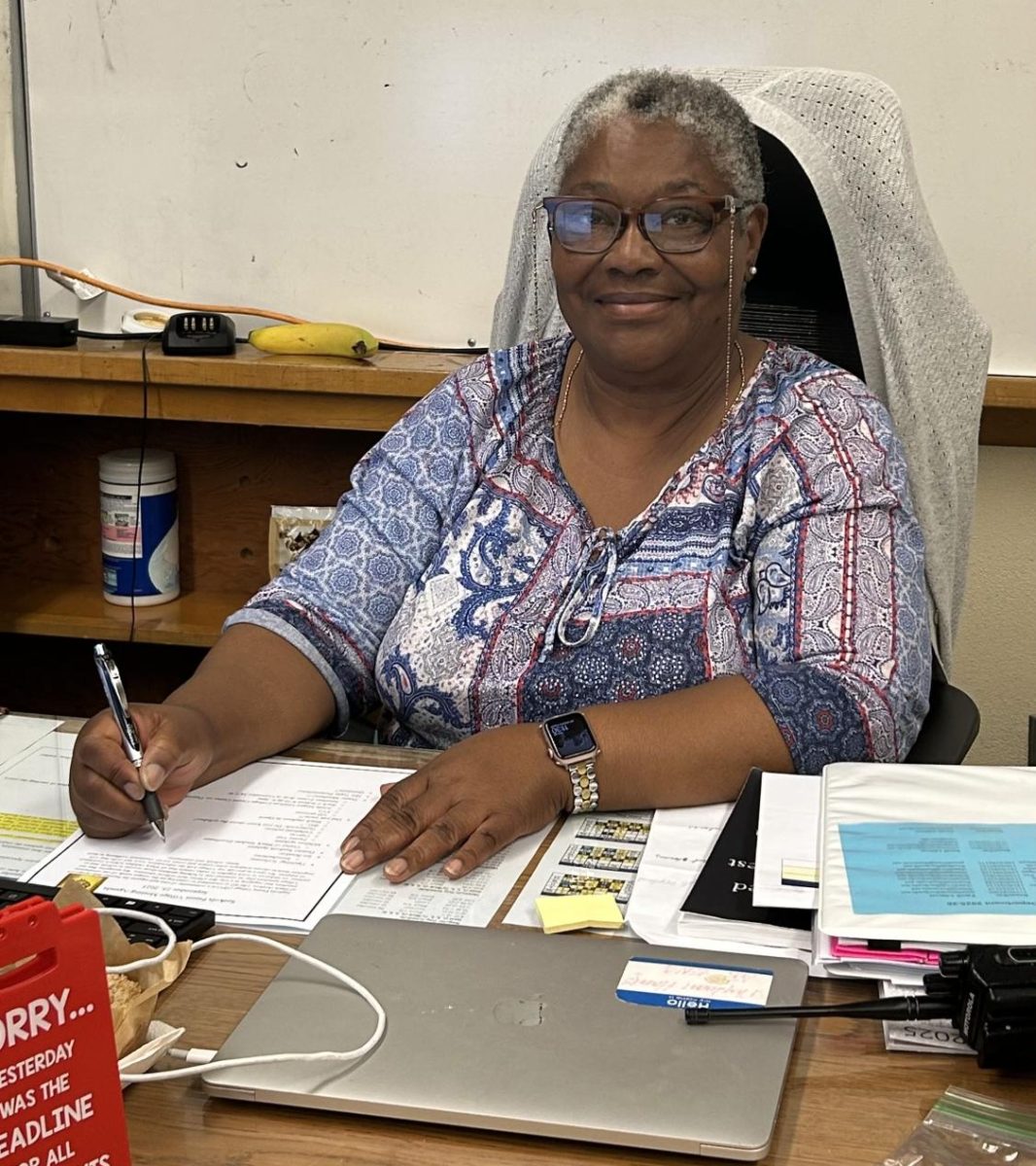
Allyson Garcia, the Millikan Cafeteria head supervisor strives to establish a safe-space for anyone self-conscious over their food intake, “I want students to know that you are welcome here and are not judged whatsoever. We will always be happy to serve and provide a place to eat guilt-free.”
Healing is not linear; developing an eating disorder does not happen overnight, nor does overcoming one. At times it may feel loud, or even impossible—but to leave you with one thing that is proven, recovery is possible.

























Zarina June Verceles • Mar 13, 2025 at 2:25 pm
On March 3, 2025, Ian Henriquez wrote an article titled “Eating Disorder Awareness Week 2025”. In this article, Henriquez brings light to his audience about the psychological condition called “eating disorders” and ways to go about the issue. To open his writing, Henriquez introduces the yearly Eating Disorder Awareness Week, which takes place from February 24 through March 2. This week takes place to recognize those who are struggling and fighting with the disorder. Throughout the rest of the article, he explains how there are many different types of eating disorders and how they have the ability to affect anyone. To conclude his article, he gives insight on the most effective ways to help someone who may be struggling with an eating disorder, also providing links to find professional help and hotlines.
One thing I really enjoyed about Henriquez’s writing is how he brought attention to the fact that there is more than one type of eating disorder. While many people know about anorexia nervosa, the category of eating disorder which drives people to starve themselves or force weight loss, there are many other categories which are just as harmful. However, these types of eating disorders are not as widely talked about as much as anorexia nervosa, so it was very nice to see awareness brought to the types such as bulimia nervosa and binge eating disorder.
Another thing that I really liked about this article is how he provided a very helpful way to approach someone who could have an eating disorder. As well as things to say to someone who may have an eating disorder, he also covered things that probably should not be brought up to them. Having the addition of things to avoid saying is very helpful to avoid uncomfortable moments or possibly triggering someone’s condition even further.
The publication of Henriquez’s article was very important and included very critical knowledge about eating disorders. His writing has many purposes; it serves as a good introduction to eating disorders for those who may be hearing about it for the first time, as well as honoring the awareness week in his own, beneficial way.
Sophia Orbiso • Mar 6, 2025 at 1:50 pm
On March 3, 2025, Ian Henriquez wrote an article titled “Eating Disorder Awareness Week 2025.” This article illustrates the importance of eating disorders which can affect people negatively. The Eating Disorder Awareness Week occurs on February 24 through March 2, it helps bring awareness to those who have suffered from this psychological condition. Henriquez expresses that almost “28.8 million North American” will suffer from an eating disorder in their lifetime. It is astonishing to know that millions of people around the globe can struggle with this horrible psychological condition, which can affect them mentally and physically. I deeply admire how Henriquez teaches the audience on how to approach people who have an eating disorder. Utilizing “I” when talking to someone with this disorder can make the person feel like they are supported, and that you are there for them. Although, as much as you want to help the person get through with this condition, it is vital to get professional help from doctors who will know how to help the patient even more. All in all, it’s important to bring awareness to this disorder as it can affect anyone, even your loved ones.
Fabian Sourinthone • Mar 6, 2025 at 9:36 am
On March 3, 2025, Ian Henriquez wrote an article titled, “Eating Disorder Awareness Week 2025”. This article brings light to the time span of February 24 through March 2 as Eating Disorder Awareness Week which helps to bring awareness to the general public about this psychological condition that can slander our own relationships with food. Henriquez gives a statistic from the Nation Eating Disorder Association, stating that the 9% of the United States population will eventually develop an eating disorder in their lifetime which is equivalent to 28.8 million people. He then continues to elaborate that eating disorders aren’t exclusive to one specific group but rather, target everybody through different eating disorders such as anorexia nervosa or bulimia.
Towards the closure of this article, Henriquez uses an empathetic view and uses sentences typically beginning with “I” to show the audience that we can be the most helpful person to an eating disorder victim and be the most supportive as well. Overall, Henriquez’s article is very informative and open, which allows the audience to view the subject from a more empathetic perspective. Using a variety of vocabulary strengthens Henriquez’s information on Eating Disorder Awareness Week which is February 24 to March 2.
Delila Perez • Mar 5, 2025 at 3:05 pm
On March 3, 2025 the article “ Eating Disorder Awareness Week” was published by Ian Henriquez. This article briefed the audience about the week of February 24 to March 2 being “Eating Disorder Awareness Week.” This article gave light to the more praised and looked-over disorder as being a harmful disorder which can come in a multitude of sizes ranging from bulimia and anorexia to binge eating. He goes on to give advice on how to speak to family who you are concerned about possibly having an eating disorder. He believes that using I statements will further make the person struggling feel validated and want to speak up about their issue. He then continues to tell the audience that they do not have to be heroes, they just need to be there and make sure that their family member or friend is validated and feels safe. He ends this article with a fact stating “ recovery is possible.” This further made me believe that Ian Henriquez is a very empathetic and caring person due to him wanting to tell the audience that if they are struggling they can recover. He has already without knowing given hope to whoever reads this article.
Danielle Haskell • Mar 5, 2025 at 3:04 pm
On March 3, 2025, Ian Henriquez wrote an article titled “Eating Disorder Awareness Week 2025”. Henriquez utilizes his article to bring attention to one of the most common yet debilitating diseases in the present day. He brings up a shocking statistic that 28.8 million Americans will experience the disorder in their life. Additionally, he politely acknowledges that eating disorders are not all the same type nor have the same effects on every victim. He explicates the vital importance of caring for those with the disorder and ways that we can support them such as using the term “I” in order to reflect a genuine care that comes from the interpersonal relationship that is shared between two.
I believe Henriquez should have explained slightly more on behalf of the Awareness week itself; its origins, impact, and implementation into society in addition to the description of the disease which is necessary for audience members who have never gone through it to get a fraction of an understanding. However, he beautifully encapsulates the pain and struggle of this psychological disorder, bringing in Millikan cafeteria head supervisor Allyson Garcia’s quote to promote the school’s care and authentic concern for students and their healing.
Haley Sawday • Mar 5, 2025 at 1:25 pm
On March 3, 2025, Ian Henriquez wrote an article titled “Eating Disorder Awareness Week 2025”. This article highlights the week of Feb. 24 through Mar. 2, as annual Eating Disorder Awareness Week, bringing awareness to the psychological condition that stigmatizes a person’s relationship with food. Henriquez mentions how 28.8 million Americans will experience an eating disorder at least once in their lifetime. He puts emphasis on the importance of approaching someone struggling with a clear plan in order to not overwhelm them. By having an empathetic approach and using statements including “I”, you are able to act as a guiding light to someone experiencing an eating disorder.
Henriquez’s article is very concise and informative, allowing the audience to completely understand the subject of concern. He uses a wide range of vocabulary and continues with a clear life of reasoning throughout. Henriquez’s technical understanding of writing allows the reader to learn and absorb information without being overwhelmed or confused.
Salma Cortes • Mar 5, 2025 at 9:41 am
On March 3, 2025, Ian Henriquez wrote an article titled “Eating Disorder Awareness Week 2025”. In this article, Henriquez informs the audience that between February 24 and March 2 is the annual Eating Disorders Awareness Week and what we can do to show our support for those struggling with eating disorders. He begins by stating the astronomical statistics of eating disorders in our country: 9% of the U.S. population will eventually face the challenge of an eating disorder, or 28.8 million North American lives can be put in jeopardy of an eating disorder. He continues by expressing how eating disorders aren’t limited to one specific group of people; rather, they target people of different ages, genders, races, and body sizes through different eating disorders, whether it’s binge eating or bulimia. A the end of this article, Henriquez states a call to action for those assisting individuals with eating disorders by emphasizing the word “I” when referring to their eating habits, and providing resources for those struggling with eating disorders such as the NEDA (National Eating Disorder Association) and the Alliance for Eating Disorders. Ian Henriquez’s choice to write about this topic is praised because many people are unaware of the support that they have and choose to go through these challenges alone.
Payton • Mar 5, 2025 at 9:28 am
On March 3, 2025, Ian Henriquez wrote an article titled “Eating Disorder Awareness Week 2025” which shed light on a mental health issue often praised or overlooked in today’s society. He wrote about what types of eating disorders exist and how we, as friends or family, can aid someone in recovery. I admire Ian’s approach of reaching out and giving comfort to those reading, while also teaching empathy within his writing. He achieves this by adding a quote from Allyson Garcia, the Millikan Cafeteria head supervisor, where she explains that she attempts to welcome those who have trouble with their relationship with food, creating a safe space within the cafeteria. Further, Ian recognizes that healing from an ED is an extremely complicated process, with many complex steps toward recovery, which many often overlook. Shedding light on eating disorders is extremely important in a society that glorifies “sick” bodies, rather than helping people achieve health and happiness in themselves. Overall, I believe that Ian’s writing showcased empathy towards those dealing with the disorder, and should be used as an example of how to bring awareness to a controversial and deeply important topic.